Introduction:
The incidence of many types of leukemia increases with age. Intensive induction chemotherapy containing cytarabine and an anthracycline has been part of the upfront and salvage treatment of AML for decades. Regimens for the treatment of ALL are also often anthracycline-based. Anthracyclines are associated with a significant risk of cardiotoxicity including anthracycline-related left ventricular dysfunction. Comprehensive baseline evaluation of cardiac function and risk may lead to better risk stratification and selection of patients who are best suited to anthracycline-based therapy. With the advent of more effective, yet less chemo-intense regimens for the management of older or unfit adults with leukemia, for example hypomethylator and venetoclax-based combinations, which gained widespread use with their accelerated approval in November 2018, one would hypothesize decreased rates of cardiovascular complications associated with the treatment of adult leukemia. To further investigate this hypothesis, we performed a nationwide analysis for adults age 25 and older with leukemia of all types and their associated cardiovascular disease related mortality.
Methods:
We utilized the Wide-ranging Online Data for Epidemiologic Research from the CDC. Patients were identified using ICD codes: C91 (Lymphoid leukaemia, C92 (Myeloid leukaemia), C93 (Monocytic leukaemia), C94 (Other leukaemias of specified cell type), and C95 (Leukaemia of unspecified cell type) with an underlying cause of death I00-I99 (Diseases of the circulatory system). Data was reviewed between 1999 to 2020 and included patients who were aged ≥25. We analyzed the age adjusted mortality rate (AAMR) per 100,000 people and stratified the data by sex, race/ethnicity, and geographical location within the USA by census region.
Results:
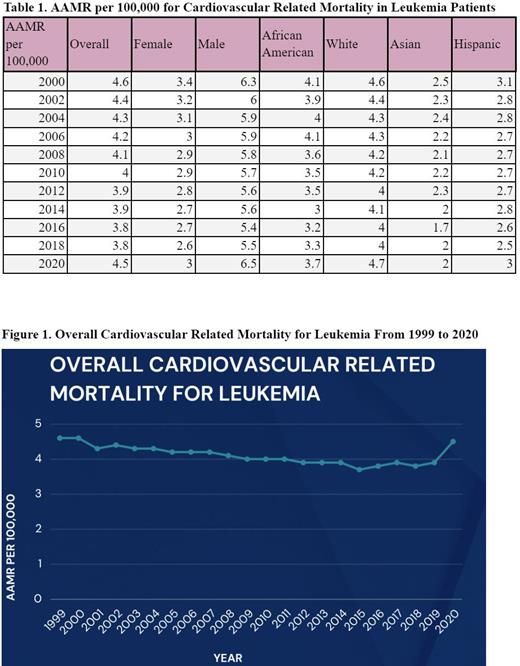
There were a total of 19,368 cardiovascular related deaths in leukemia patients between 1999 and 2020. There has been a decreasing trend in overall mortality associated with cardiovascular diseases from 1999 to 2019, falling from 4.6 to 3.9 deaths per 100,000 people, with an annual percent change of -2.89% (Figure 1). Both sexes mirrored this trend, with female mortality rates improving from 3.4 to 2.7 (APC -3.26%) and male rates from 6.5 to 5.6 (APC -3.07%) between 1999 and 2019. In 2020, it was observed that leukemia patients had an increased cardiovascular related mortality: 4.5 AAMR overall, 3.0 AAMR in females, and 6.5 AAMR in males . There was not a statistically significant difference in mortality changes by race (Table 1).
Conclusion:
Our study reveals a decrease in mortality rates from cardiovascular disease in leukemia patients from 1999 to 2018 followed by a relatively sharp increase noted in 2020. The steady improvements noted from the early 2000s to the 2010s may be attributable to awareness of known toxicities that led to enhanced screening and active monitoring for cardiovascular complications. Electrocardiograms, echocardiograms, and cardiotoxic markers including troponins and natriuretic peptides have served as diagnostic and risk-stratification tools. In 2020 leukemia patients exhibited a sudden increase in mortality across all sub-groups. One may postulate that this is related to COVID-19-related complications/delays in treatment, however, another possible explanation may be incompletely recognized toxicities of novel therapeutics. Interestingly, preclinical data have demonstrated that venetoclax treatment resulted in cardiac damage as evidenced by major changes in histopathology and markedly elevated cardiac enzymes and hypertrophic genes markers. Moreover, a drastic increase in oxidative stress, as well as inflammatory and apoptotic markers, with a remarkable decline in the levels of Bcl-2 has been observed (AlAsmari et al Int J Mol Sci 2022). Clearly, continued monitoring and further exploration is needed to identify the reason or reasons for the noted 2020 phenomenon. Continued data collection in the post-Covid vaccine era is likely to help to further elucidate the reasons for the unexpected uptick in cardiovascular-related morbidity and mortality in our leukemia patients.
Disclosures
Koprivnikar:Alexion: Consultancy; GSK: Consultancy; Novatis: Consultancy; Apellis: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal